6 Misconceptions that Increase Your Risk of Heart Disease

According to the CDC, heart disease is the leading cause of death in the U.S., accounting for almost one in every four deaths. Although heart disease is sometimes thought of as a “man’s disease,” around the same number of women and men die each year of heart disease in the U.S. Yet, many Americans don’t know that. Our recent survey found that many Americans don’t know a lot of things about Heart Disease and Heart Attack prevention.
1. Cancer Is the Leading Cause of Death in the U.S.
38% of Americans who responded to our recent survey about Heart Health agree with this statement: “cancer is the leading cause of death in the U.S.” 30% aren’t sure.
Before 1910, Americans were more likely to die from Tuberculosis, Pneumonia and Influenza than anything else. “Diseases of the Heart” took the top spot in 1910. Today, Heart Disease is still the #1 cause of death in the U.S. Cancer is #2.
2. Heart Attacks Run In My Family—Nothing I Can Do About That
Some people are destined to have a heart attack due to family history and there’s very little they can do to prevent it. 21% of our survey respondents believe that statement is true. 24% say they’re not sure.
The correct answer: You may indeed be at increased risk if you have a family history of heart attack, i.e., your siblings, parents or grandparents had early heart attacks but increased risk does not mean inevitable! Harvard Health reports that “while you cannot escape your family genes, it is possible to stay ahead of them.”
Besides taking steps to reduce your risk, such as adopting better eating habits, staying physically active and eliminating smoking, there are medical tests that can help gauge the health of your heart and arteries.
According to Harvard Health: A blood test can look for certain biomarkers in the bloodstream, like elevated levels of lipoprotein(a), a lipid particle similar to low-density lipoprotein (LDL), which is linked to cardiovascular risk and is largely determined by genetics. A coronary calcium scan can detect specks of calcium in the walls of the arteries, which offer an early sign of heart disease. “This test is often used for people who are at a moderate risk of a heart attack and can help identify people who may be candidates for preventive medicines,” says Dr. Pradeep Natarajan, a cardiologist at Massachusetts General Hospital.
3. I’m In Great Shape, So…
WATCH: “It is so important to know your health… There were things going on inside my body that I needed to be more aware of.” –@MyTrainerBob pic.twitter.com/6cgaoG0aWS
— TODAY (@TODAYshow) April 4, 2017
While some may believe they’re destined for a heart attack because of family history, Bob Harper, a trainer on the TV show “The Biggest Loser” did not. Harper knew that he had a family history of heart disease—his mother died of a heart attack. But, he lived a very healthy lifestyle and says he worked out “all the time.” Harper suffered a near-fatal heart attack at age 51. In an interview on the “Today” show, he said, “It was hugely shocking for me. I’ve learned a lot about myself. I’ve learned a lot about the fact that genetics played a part in this. It is so important to know your health.” Harper encouraged others to get regular check-ups even if they are dedicated to fitness like him.
Daniel Edmundowicz, chief of cardiology at Temple University Hospital says that Harper’s heart attack appears to be the type that comes with no warning—instead of a gradual narrowing, the built-up plaque ruptures. The most common result is sudden death.
Harper discovered that healthy lifestyle may not be enough to counter a family history of heart disease. “Go to the doctor, get your cholesterol checked, see what’s going on in the inside so it doesn’t happen to you what happened to me,” he says.
58% of people who responded to our survey believe that strenuous exercise can cause a heart attack. 27% say they’re not sure.
4. Exercise Can Cause a Heart Attack
Harper, an exercise fanatic, suffered a massive heart attack after a completing a crossfit class so…you could conclude that exercise was the culprit. It wasn’t. According to Mayo Clinic cardiologist Dr. Sharonne Hayes, “All heart attack patients have had an underlying condition that caused the attack.”
Neel Chokshi, medical director of the University of Pennsylvania’s sports cardiology and fitness says, “The long-term benefits of exercise outweigh the slight increased risk during acute exercise…any exercise regimen should begin slowly and increase gradually, letting the heart – and the rest of the body – build strength. If you exercise and do have a heart attack, you are more likely to bounce back and less likely to have complications.”
A 2015 study found that for the 35-to 65-year-olds who had sudden cardiac arrests, only 5 percent happened during a sports activity. That means 95 percent of them happened while not working out.
5. No Chest Pain… Can’t Be a Heart Attack
30% of our survey respondents believe that a person having a heart attack will always have some degree of chest pain or discomfort. 15% aren’t sure. Chest pain is the most common symptom, but many heart attack patients don’t experience any chest discomfort at all.
Women are somewhat more likely to have shortness of breath, nausea and vomiting, unusual tiredness (sometimes for days), and pain in the back, shoulders, and jaw. An Atherosclerosis Risk in Communities (ARIC) Study has found that almost half (45%) of heart attacks appear to be clinically silent — that is, not associated with any symptoms at all, at least that the patient can recall.
The Hollywood version of a heart attack—a man grabbing his chest and falling to the ground—is not an accurate portrayal of what people typically experience.
6. Headaches, Dizziness and other Symptoms are Indicators of High Blood Pressure
Our survey respondents were given a list of symptoms and asked to indicate which they believe are signs of high blood pressure. 82% believe that people with high blood pressure will experience dizziness and 76% will experience headaches.
Most people with high blood pressure will not experience any symptoms—the only way to know if you have high blood pressure is to have your blood pressure tested.
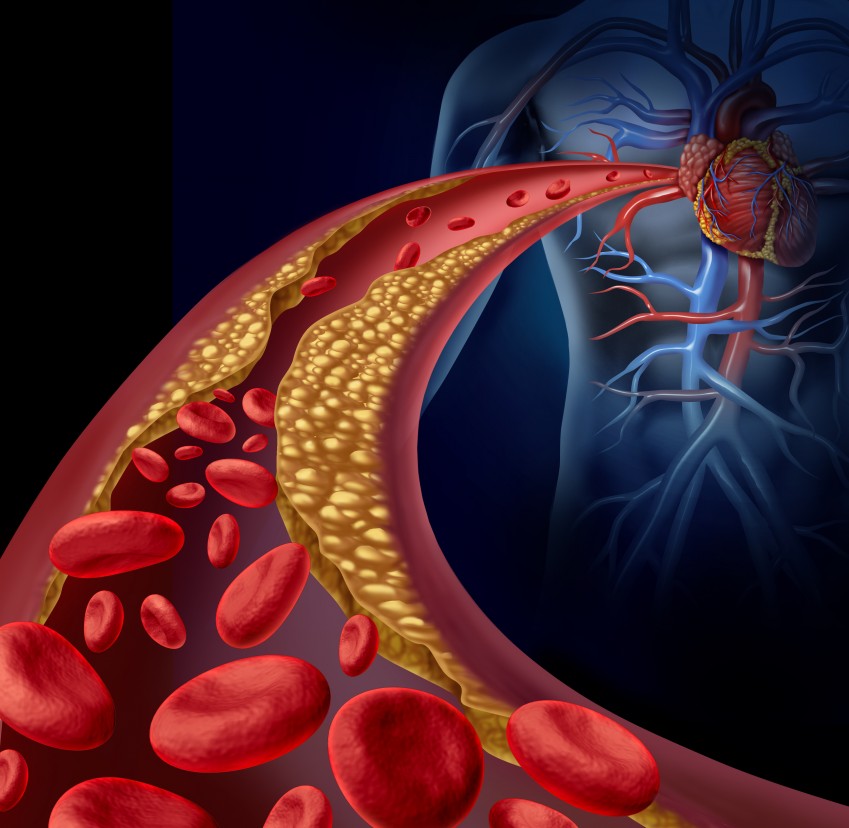
Everyone should know their blood pressure numbers, because, according to the American Heart Association: High blood pressure is a largely symptomless “silent killer.” If you ignore your blood pressure because you think a certain symptom or sign will alert you to the problem, you are taking a dangerous chance with your life. The excess strain and resulting damage from high blood pressure causes the coronary arteries serving the heart to slowly become narrowed from a buildup of fat, cholesterol and other substances that together are called plaque. This slow process is known as atherosclerosis. As arteries harden with plaque, blood clots become more likely to form. When an artery becomes blocked due to an accumulation of plaque or a blood clot, the flow of blood through the heart muscle is interrupted, starving the muscle of oxygen and nutrients. The damage or death of part of the heart muscle that occurs as a result is called a heart attack.
The symptoms on the list could be symptoms of other health conditions and should be evaluated by a doctor.
Conclusion
At some point in your lifetime, you will have an increased risk of heart attack. Even if you somehow manage to avoid all of the risk factors (which is nearly impossible) men age 45 or older and women age 55 or older are more likely to have a heart attack than are younger men and women. Heart disease prevention includes regular screenings for high blood pressure and high cholesterol; without testing for them, you probably won’t know whether you have these conditions.
The Mayo Clinic advises the following:
- Blood pressure. Regular blood pressure screenings usually start in childhood. You should have a blood pressure test performed at least once every two years to screen for high blood pressure as a risk factor for heart disease and stroke, starting at age 18. If you’re age 40 or older, or you’re between the ages of 18 and 39 with a high risk of high blood pressure, ask your doctor for a blood pressure reading every year. Optimal blood pressure is less than 120/80 millimeters of mercury (mm Hg).
- Cholesterol levels. Adults should generally have their cholesterol measured at least once every five years starting at age 18. Earlier testing may be recommended if you have other risk factors, such as a family history of early-onset heart disease.
Based on your numbers, your doctor will be able to determine the need for further tests and medications.