Mammography Screening at 30 Beneficial for Some Women

The current American Cancer Society guidelines suggest that women ages 40 to 44 could undergo mammograms every year if they want to, and that women ages 45 to 54 get mammograms every year. Many professional groups, including the Radiological Society of North America (RSNA), recommend beginning routing screening at 40. Recommendations for younger women are less clear.
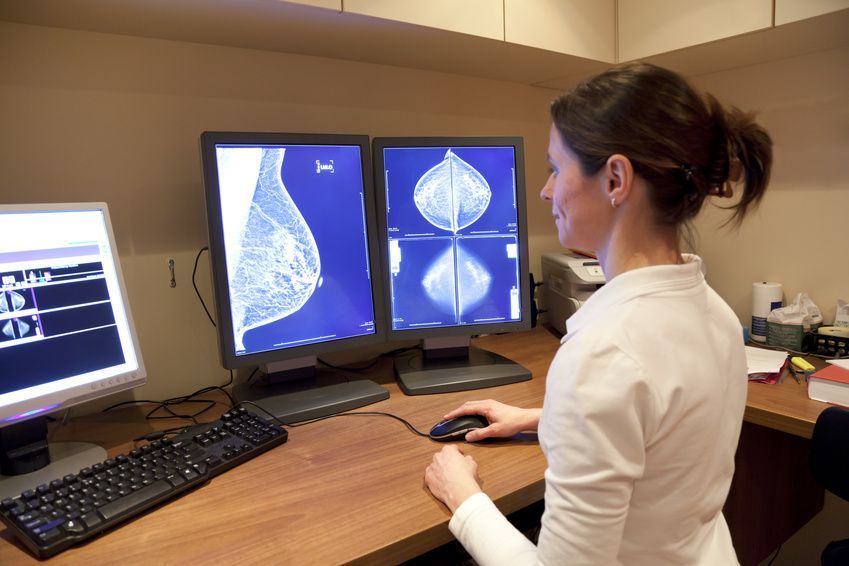
A new study of more than 5 million mammogram outcomes found that yearly breast cancer screening with mammography beginning at the age of 30 might benefit women with certain risk factors. Mammography is the standard imaging test for breast cancer. Based on the results of mammography, doctors may call a patient back for more care and recommend a biopsy.
The results of the study show that annual mammography beginning at age 30 might benefit women who have at least one of the following risk factors: dense breasts, a personal history of breast cancer, or a family history of breast cancer.
Current Focus and Guidelines for Mammography
Until recently, researchers have not focused their attention on breast cancer screening in women under the age of 40. This is primarily because most women in that age range do not get mammograms. Unfortunately, some younger women have an increase risk for breast cancer – and an increased need for earlier or supplemental screening.
For this study, researchers used data from the National Mammography Database (NMD), which is the largest database of screening mammography outcomes in the United States. The database contains data from more than 19 million mammograms, including mammography interpretations and biopsy results.
The research team analyzed information for more than 5.7 million mammograms done on more than 2.6 million females over an 8-year period in 150 facilities across 31 states. The 8-year study period extended between January 2008 and December 2015. The researchers compared the screening in women between the ages of 30 and 39 who had one of the three specific risk factors with women age 40 to 49 without those risk factors.
The group of researchers calculated four performance metrics for each patient age and risk group: cancer detection rate, recall rate, and the rates of biopsy recommendations and biopsy performed. The cancer detection rate reflects the percentage of cancers found on mammogram, while the recall rate is the proportion of people called back for follow-up testing after mammogram screening.
Medical professionals use risk prediction models to predict the probability that someone will develop a health problem, based on that person’s risk factors. Some of the most commonly used models for breast cancer incorporate a number of different risk factors. The Gail Model, for example, uses personal information such as a woman’s age at the start of menstruation and the number of previous biopsies to determine risk.
Because they use different data for analysis, different models can come up with different results, which can be confusing for both patients and doctors. In fact, the researchers note that breast density is an important risk factor for breast cancer, but only one current risk model includes it.
The findings
The research team compared screening performance metrics among the different groups of women based on the participants’ age, breast density and risk factors. They found that the group of younger women with the three risk factors had similar cancer detection and recall rates as did the older women without the risk factors.
For this study, the researchers evaluated the three specific risk factors:
- Family history of breast cancer that involved any first-degree relative of any age
- A personal history of breast cancer
- Having dense breasts
Focusing on just these three risk factors allowed the doctors to define “increased breast cancer risk” in a simpler, more inclusive way. By this definition, any woman with one of these three risk factors has an increased risk of breast cancer, regardless of her age. The researchers found that some of the participants under the age of 40 had increased risk of breast cancer because they had dense breast tissue, a family history or a personal history.
The researchers categorized the participants by age and compared cancer detection rates, recall rates and biopsies. Women in the 30 to 34 age group and women in the 35 to 39 age group had similar rates of cancer detection, recalls and biopsies. Most strikingly, though, the researchers found that women in their 30s with at least one of the three risk factors had the same or similar cancer detection rates and recall rates as women ages 40 to 44 with average risk.
In other words, the study suggests that women in their 30s who have dense breast tissue, a personal history of breast cancer or a family history of breast cancer have the same risk of breast cancer as older women without those risks, and that they may want to consider annual mammography.
“Women with at least one of these three risk factors may benefit from screening mammography beginning at age 30, instead of 40,” said Cindy S. Lee, M.D., assistant professor of radiology at NYU Langone Health in New York City and lead author of the study. The researchers presented their results at the RSNA’s annual meeting.